By the time I was born into the virological soup of suburban Melbourne in 1960, the last Australian polio epidemic was behind us and the remaining childhood diseases were vying for most-feared status. Scarlet fever and diphtheria had gone and rheumatic fever was fast receding. For my parents, measles had taken on the mantle of the “bad” (if routine) childhood illness. Measles made you feel terrible and its complications could be severe.
Most kids contracted the illness by the age of six, so they had little personal memory of it, but their parents certainly witnessed the distress it could cause. My measly memory is of lying in a darkened bedroom listening to the hushed conversation of my mother and our GP outside the door. I was six or seven at the time and I later learnt that I was a bit delirious and my mother was worried that I had developed one of the uncommon but feared complications, encephalitis, or inflammation of the brain.
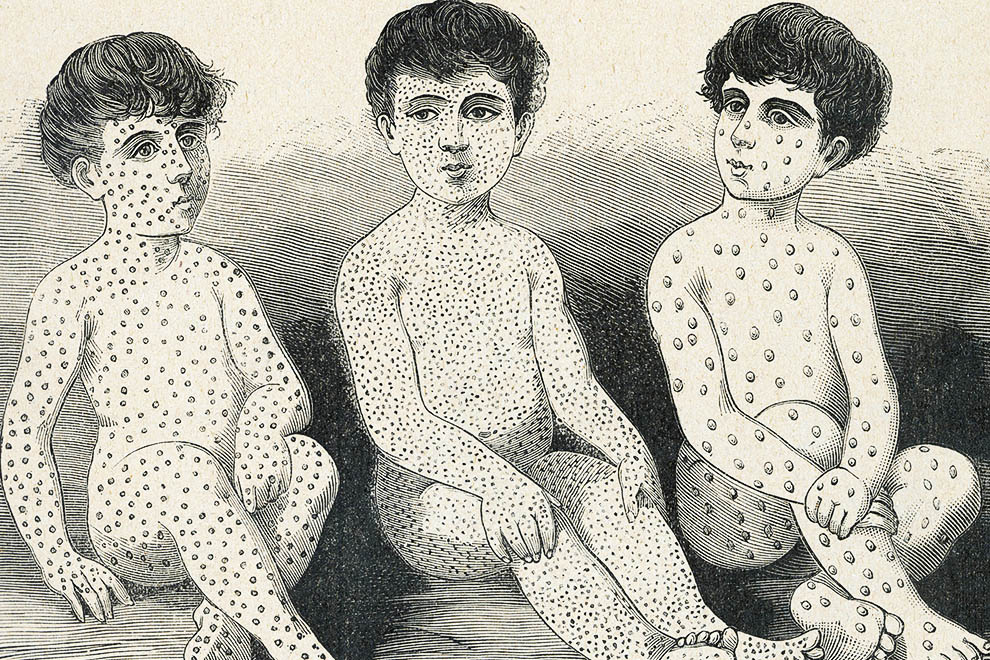
The measles virus is present in the respiratory secretions of an infected person and is transmitted to others through inhalation or contact with the conjunctivae. The virus multiplies in the nose, throat and airways of its new host who, with each cough and splutter, launches viral particles into the air in aerosols. The virus can persist in a room for two hours after an infected person leaves. It usually takes ten to fourteen days after exposure (the range is six to twenty-one days) for the first signs of the disease to appear. These are known as the prodromal symptoms and include fever, tiredness, irritability, cough, runny nose and conjunctivitis. Two to four days after the prodrome commences, a striking rash appears, usually beginning behind the ears and spreading across the face and neck and then progressing to cover the entire body. The rash starts as small, discrete, slightly raised, red blotches but eventually these may all join up into one confluent rash.
Very few doctors who graduated after 1980 will have seen a real patient with this clinical constellation, and it is not uncommon for a case of measles to be misdiagnosed as a drug reaction (which is the most likely explanation for a measles-like rash in countries where vaccination rates are high). About 30 per cent of measles cases lead to complications, the most common being diarrhoea, otitis media (middle ear infection) and pneumonia. Encephalitis is much rarer (about one in 1000 cases) and the rare but devastating long-term sequel known as SSPE usually appears seven years after the initial illness. SSPE produces a progressive neurological deterioration that affects behaviour, intellect and movement and is universally fatal. I saw one case in 1982 when I was a student but it has now all but disappeared in the developed world.
If you are an Australian reader older than forty-eight, then you can be 97 per cent confident that you had measles as a child. If you are younger than that, then it is still highly probable that you are immune, but the more youthful you are the more likely your protection will be due to vaccination rather than to a “natural” infection. Vaccination is a victim of its own success – contemporary measles vaccine coverage in the developed world is such that a disease that was once a near-ubiquitous rite of childhood passage is no longer part of the received wisdom of twenty-first-century mothers and fathers. The fading folk memory of infectious diseases has allowed the specious arguments of the anti-vaccination lobby to gain considerable traction among anxious young parents. If you listen to the propaganda of the “anti-vaxxers,” you would wonder what the fuss about the disease was in the first place. One zealot has even produced a children’s picture book that extols the virtues of “natural” measles infections.
So why should we worry about measles? Obviously a disease that affected nearly 100 per cent of the population must have had a relatively low fatality rate or there wouldn’t be so many of us baby boomers. In the mid-twentieth-century United States, for example, the measles case-fatality rate was less than 1 per cent (in other words, fewer than one in a hundred children who contracted the disease died). By 1990 the rate had fallen to around 0.05 per cent, or five in 10,000.
But the raw numbers can be striking. In Victoria, for instance, between 600 and 800 children were hospitalised during each of the state’s four major measles epidemics between 1960 and 1970, and 146 deaths were attributable to measles over roughly that period.
The fatality rates of measles fell across the West during the twentieth century, probably as a result of better nutrition and improvements in health services. But measles remains a dreaded and deadly disease in the developing world. There, the case-fatality rate ranges from 0.5 per cent to 6 per cent depending on the region, and during war and famine it can approach 30 per cent. Despite remarkable gains made over the past thirty years because of vaccination, the World Health Organization, or WHO, estimates that 114,900 measles sufferers died worldwide in 2014.
In 1954 an eleven-year-old boy named David Edmonston contracted measles in his boarding school in Boston, Massachusetts. At the time, virologist John Enders (who won a Nobel prize for work that led to the polio vaccine) was scouring the local residential institutions in search of measles virus samples. After dozens of failed attempts with other patients, Enders was able to grow measles from a swab that he took from David’s throat. Over several years he cultivated the virus in his laboratory, allowing it to become weaker with each passage through the cell culture. This “attenuated” strain was successfully tested as a vaccine in monkeys and then in humans. The first to receive the vaccine were severely disabled children with conditions such as Down syndrome, microcephaly and cerebral palsy, who were living in an institution in Massachusetts. In a move unusual for the 1950s, the researchers obtained written consent from the parents of each child before administering the vaccine. The results were remarkable: all of the vaccinated children were protected from measles during the next outbreak.
In 1963, after further studies confirmed its safety and effectiveness, the Edmonston strain was used in the first US measles vaccine. Within a decade the annual number of cases fell from several million to several thousand, an effect that was seen in every country where the vaccine was rolled out. Even in the developing world the number of cases fell dramatically. During 2000–14, the number of annually reported measles cases worldwide decreased by 69 per cent and it has been estimated that 17.1 million deaths were prevented by measles vaccination during that same period.
Even as the collective memory of the disease’s severity faded, the safety of the measles vaccine was never brought into question – not, at least, until a paper was published in theprestigious medical journal The Lancet in 1997, suggesting that autism was linked to the measles, mumps and rubella, or MMR, vaccine. This work was subsequently shown to be scientifically invalid and the lead author, Andrew Wakefield, was deregistered by Britain’s General Medical Council, which ruled that he had acted unethically and shown a “callous disregard” for the children involved in the study. Since then, carefully conducted, large-scale studies across the world have failed to show any association between MMR and autism, yet by 2004 measles vaccination rates in Britain had fallen to 80 per cent and measles cases had skyrocketed. Modern confidence in vaccines is very fragile and it took ten years for coverage to return to the levels seen before the autism scare.
Despite this setback, in March 2014 the WHO announced that measles had been eliminated from Australia, though the news didn’t make much of a splash in the media. Indeed, in light of stories about measles outbreaks in returned travellers and groups with anti-immunisation views, many readers would have been puzzled by the announcement in the first place. If outbreaks still occur, how can the disease be “eliminated”? It’s all a matter of definition. Elimination means local transmission of a disease has ceased, but it doesn’t mean that the disease can’t be reintroduced from countries that haven’t eliminated it. Eradication, on the other hand, would mean there were no more cases of measles anywhere in the world. Only one human disease – smallpox, in 1980 – has ever been eradicated (although the global eradication of polio is tantalisingly close). Dozens of countries have achieved measles elimination but eradication is not currently on the WHO agenda.
To understand why, we need to understand herd immunity: the indirect protection that a non-immune individual receives from the immune members of the same population. The proportion of the “herd” that needs to be immune varies between diseases. For some, a surprisingly modest proportion needs to be immune to stop an epidemic from occurring. Only around 80 per cent of the population needed to be vaccinated against smallpox to achieve global eradication and only around 60 per cent vaccination coverage would be required to protect against a pandemic swine flu epidemic. How high does it have to be for measles?
You can determine the threshold for population immunity once you have established how many secondary infections one infected person produces. This is known as the reproductive number, or R0. (R0 is one of the most useful numbers in infectious diseases, so even if you are maths-phobic stay with me for another three paragraphs). If R0 is less than 1, then the disease will disappear; if it is greater than 1, there will be an epidemic. The more contagious the infection is, the more likely that R0 will be higher. (Contagiousness is just one of many factors that need to be considered in calculating R0, but here I will restrict my discussion to this key factor.) The degree of contagiousness varies considerably from one infection to another: most forms of leprosy are hardly contagious at all, for instance, so R0 in almost every population is less than 1; Ebola requires direct contact with infected blood or bodily secretions so it was relatively easy to reduce R0 below 1 once appropriate infection control was instituted during the 2014–15 epidemic. Even influenza is less contagious than most people think; the pandemic swine flu of 2009 had an R0 between 2 and 3; smallpox was about 5. But measles is probably the easiest infection on the planet to pass from one person to another – its R0 is between 12 and 20.
Once you have calculated R0, a simple piece of arithmetic produces the proportion of people who need to be immune to achieve herd immunity. This is known as the herd immunity threshold, or HIT. The HIT is 1–1/R0.
For smallpox, where R0 = 5, the HIT = 1 minus 1/5 = 4/5 = 0.8 or 80 per cent.
For measles, where R0 =15, the HIT = 1 minus 1/15 = 14/15 = 0.933 or 93.3 per cent
So, to achieve local measles herd immunity, more than 90 per cent of the population has to be immune. For eradication, this would have to be repeated everywhere across the globe. It seems achievable: in 2015 the average level of vaccine coverage in Australia for five-year-olds was an impressive 93.7 per cent. Unfortunately, this does not mean that all those children are, or will remain, immune. While natural infection with measles confers lifelong immunity to nearly 100 per cent of those affected, measles vaccine is between 90 and 95 per cent effective at inducing immunity – and this may wane over time. Therefore the vaccine coverage required to reach the HIT has to be greater than the 93.3 per cent we calculated above. If we generously assume 95 per cent vaccine efficacy, the actual proportion of the population that must be vaccinated is 93.3 per cent x 1/95 = 98.2 per cent, a level that has never been achieved in Australia. With the current vaccine it may be that eradication is simply not a reachable goal.
Herd immunity reminds us that vaccination is not purely a self-interested act but also one of altruism and comity. I believe that a modern society has a duty to achieve herd immunity so that it can provide protection for the small group who are unable to be vaccinated for medical reasons (those with severe impairment of their immune systems, for instance, due to congenital illnesses, cancers, HIV or organ transplantation), for those who did not respond to the vaccine and for older people whose vaccine immunity has waned over time. But the success of vaccination has resulted in a population that has been spared the powerful direct experience of measles (and other infections) and that may be more susceptible to the superficially appealing reasoning of the anti-vaccination movement. While the anti-vaxxers’ effect on vaccine coverage is probably marginal, we have seen that there isn’t much buffer in vaccine coverage rates; small falls in coverage may be all that is required for herd immunity to be lost and for a vaccine-preventable disease to re-establish itself.
I also fear for the children of the anti-vaxxers in the coming years. Denied the vaccine themselves, but temporarily protected by the herd immunity generated by their responsible neighbours, they will grow into susceptible adults who travel to countries where herd immunity for most infectious diseases is low or non-existent. There, these immunological innocents will encounter vaccine-preventable illnesses such as rubella, mumps, pertussis, chickenpox, meningococcal disease, Hib, hepatitis A and B, diphtheria and tetanus, to name just a few. And they will put the ideology and pseudoscience of their parents to the test in a natural experiment that no ethics committee would ever dare to approve. •