Tess Ryan writes:
In the waiting room of a general practice a woman sits waiting to see the male clinician. She is uncomfortable and worries, because of past experiences, whether her concerns will be taken seriously or the doctor will see her problems as trivial.
An Aboriginal person also sits uneasily, knowing that the non-Indigenous people around her have no understanding of what her life entails, or what it means to be deemed a problematic statistic, or the assumptions that dictate how her health concerns are framed. If you have kidney or liver problems, it must be due to alcohol use. If you are a diabetic, it is due to the food you eat.
Also waiting is someone with a chronic condition. This person is running through her mind the list of concerns about her body, and the next complications she may face. When some new problem arises that can’t be explained neatly within diagnostic categories, she knows from past experience that she will be told, unsatisfyingly, “This is probably just a part of your condition.”
And an academic, who writes about race, cultural nuances and systemic failures across various institutions in the hope of disrupting them for the better, also waits for the doctor.
How many people sit in that waiting room? The answer is one. Me.
I walk into a medical practice with an understanding of health systems derived from my various identities: a Black Australian, a woman, someone with a deepening chronic illness, and an academic and writer with an understanding of the denial of Black voices and how health systems ignore the totality of people’s lives.
I come with many languages, some embedded in an emotional place that echoes through my body, and a history of being told I am less. I also bring an intellectual language for describing my understanding and experiences of racism and intergenerational trauma.
Observing myself in that waiting room, I am overcome with exhaustion. These discussions about race and racism that have come to the fore with the pandemic and with Black Lives Matter are necessary. But so utterly tiring. In case you haven’t noticed, we have been doing this work for a very long time.
____________
Melissa Sweet writes:
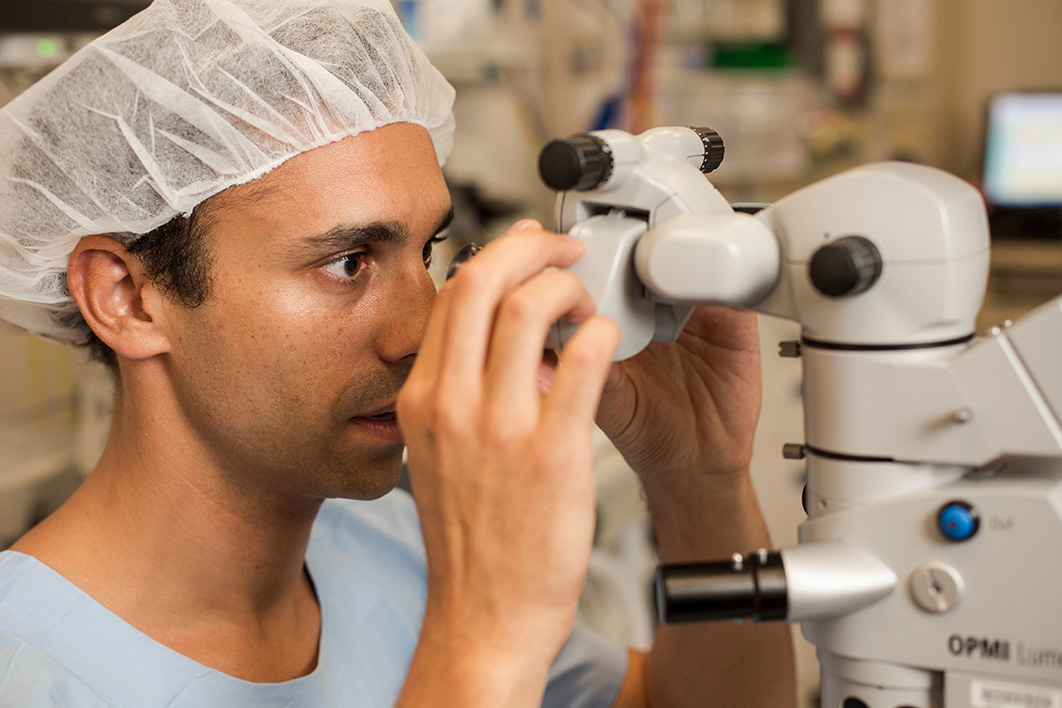
On a late spring’s evening in 2018 the Fred Hollows Foundation hosted a historic celebration in Adelaide. Guests whipped out their phones to record and tweet the beaming smile of the guest of honour, the president of the Australian Indigenous Doctors’ Association, Kris Rallah-Baker, with his arms wrapped around his parents. The celebration marked Dr Rallah-Baker’s graduation as Australia’s first Indigenous ophthalmologist.
Although he was just thirteen years old when the legendary eye surgeon Fred Hollows died in 1993, even then he had his sights set on becoming a doctor. But a careers counsellor at his school advised him against doing medicine, despite the fact that he was a top student, because “Aboriginal doctors were virtually unheard of.”
Low expectations are among the many ways that racism is expressed towards Aboriginal and Torres Strait Islander people, and Rallah-Baker experienced many other manifestations during his medical training. Not long before that graduation ceremony, he decided to put his concerns on the public record. “My own dealings with blatant racism, degradation, training delays, bullying, harassment and racial vilification are unfortunately considered an unremarkable experience amongst my Indigenous medical brethren,” he wrote in Insight, the industry magazine for the eye-care sector.
Initially the Royal Australian and New Zealand College of Ophthalmologists, or RANZCO, dismissed those concerns. But it quickly came under fire, with one headline referring to the college’s having engaged in “whitesplaining.” In an open letter, Aboriginal and Torres Strait Islander academics and health professionals, along with the Australian Indigenous Doctors’ Association and members of the Leaders in Indigenous Medical Education Network, condemned the college for “its callous disregard” of Rallah-Baker’s “experiences of racism and bullying and the attempt to publicly undermine his integrity and commitment to his profession and his people.”
Rallah-Baker had given RANZCO the chance to be part of the solution, they wrote. “We urge RANZCO to take up the call for the necessary institutional reform needed to ensure that Dr Rallah-Baker is not the first and last Indigenous ophthalmologist in this country. We urge you to listen and learn from his experiences and further, commit to action in the interests of Indigenous health justice.”
Within weeks the college issued a public apology — and Rallah-Baker is struck by how far the organisation has evolved since then. “I am absolutely impressed at how far they have come,” he tells me. “It’s been transformative for the organisation.”
He describes an increased focus on Indigenous eye health in training programs and an ambitious Reconciliation Action Plan. Aboriginal, Torres Strait Islander and Māori flags are now displayed prominently at college events, Acknowledgement of Country and other Indigenous protocols are in use, and the college has introduced cultural safety training — a strategy for tackling racism that encourages health practitioners to reflect critically on their knowledge, skills, attitudes and behaviour.
At a personal level, Rallah-Baker appreciates how RANZCO colleagues have rallied around at critical times, such as when the mining company Rio Tinto destroyed sacred sites at Juukan Gorge in Western Australia during Reconciliation Week, and when the Black Lives Matter movement brought global attention to the pervasive and violent effects of racism in all its forms.
But the point is not so much that a conservative, largely white organisation like RANZCO could change for the better. More significantly, this is just one of countless examples of how hard Aboriginal and Torres Islander people work, individually and collectively, to deal with racism — and not only in its most obvious forms.
The work has involved generations of scholarship, teaching, training, activism and advocacy. It has involved campaigning for policy and organisational change to tackle the institutional racism whereby society’s institutions and systems are designed to operate in ways that privilege some groups over others. In Australia, institutional racism is most glaringly evident in the failure of mainstream health, education, justice, media and other sectors to address the aspirations and needs of Aboriginal and Torres Strait Islander people.
Aboriginal and Torres Strait Islander people also contribute immense emotional labour in pushing for justice and change after loved ones have been harmed or killed. In her report on the death of Wiradjuri woman Naomi Williams from septicaemia at Tumut Hospital in 2016 — the result of an infection that is usually treatable — NSW deputy coroner Harriet Grahame acknowledged “the enormous pain Naomi’s family and friends feel and I thank them for their courageous attendance and dedicated participation in these difficult proceedings.”
Grahame saw their motivation as twofold: “They have been dedicated to trying to find out exactly why Naomi died, but they have also been looking for ways to improve health outcomes for other Indigenous patients in their local community. In this way they are honouring Naomi’s life and acknowledging her status as an emerging leader of her community.” Her report stresses the importance of Aboriginal people’s representation at all levels of the health system, and explores the impact of implicit bias and racism on healthcare for Indigenous patients.
Grahame documents “clear and ongoing inadequacies” in Ms Williams’s care, also finding that the care provided to her family after her death was “not compassionate or appropriate.” In the several months before she died, she presented at least eighteen times to the hospital with recurring, persistent symptoms, including vomiting and nausea, but felt her concerns were not being taken seriously because she was being stereotyped as a drug user rather than being referred to appropriate services.
The pandemic has brought the harmful impacts of racism to greater prominence, with headlines around the world reporting that Black people are not only more likely to contract Covid-19 but also more likely to die from it.
For Aboriginal and Torres Strait Islander people, however, such concerns are no revelation. Next year will mark the fiftieth anniversary of the Redfern Aboriginal Medical Service, the country’s first Aboriginal community-controlled health service. It was established to provide a culturally safe alternative to mainstream services, and since then it and other similar organisations have argued that tackling racism is critical to improving the health and wellbeing of Aboriginal and Torres Strait Islander people.
Yet these calls have fallen largely on deaf ears. In fact, the r-word doesn’t appear in three landmark documents in the history of Australian health reform: Australia: The Healthiest Country by 2020, the “roadmap for action” of the National Preventative Health Strategy (316 pages); A Healthier Future for All Australians, the final report of the National Health and Hospitals Reform Commission (279 pages); and Building a 21st Century Primary Health Care System, which spelt out “Australia’s First National Primary Health Care Strategy” (forty-four pages).
Last year saw the release of health minister Greg Hunt’s ambitiously titled but modestly scoped report, Australia’s Long Term National Health Plan to Build the World’s Best Health System (twenty-four pages), and plans for a new national preventive health strategy. Again, though, silence on this central issue.
Writing in the Medical Journal of Australia in March, University of Queensland health researchers Chelsea Bond and David Singh highlighted other omissions and pointed out that the National Health and Medical Research Council has yet to invest in a research program to understand and tackle racism in the health system.
By contrast, the National Aboriginal and Torres Strait Islander Health Plan 2013–2023, released by the government in 2013 and developed in partnership with Aboriginal and Torres Strait Islander organisations, made action against racism central, as did this year’s report from the Close the Gap campaign, which represents peak Indigenous and non-Indigenous health bodies, non-government organisations and human rights organisations. Yet the most recent of the federal government’s Closing the Gap reports mentions racism just once and contains no specific targets for tackling it, whether population-wide or in critical areas such as health, education or justice.
Among the Aboriginal and Torres Strait Islander organisations and leaders working overtime to break this silence is the Coalition of Peaks, which represents about fifty Indigenous organisations. In March, the coalition signed an historic agreement with the Council of Australian Governments setting out a power-sharing arrangement over the next decade, including a commitment to three-yearly Aboriginal and Torres Strait Islander–led reviews of Closing the Gap work.
The Coalition of Peaks is due to sign an agreement with federal, state and territory governments and the Australian Local Government Association on the next iteration of the Closing the Gap strategy. It is pushing not only for increased investment, according to its lead convenor, Pat Turner, but also for funding to go directly to Aboriginal and Torres Strait Islander–controlled organisations.
For Kris Rallah-Baker, the present moment — with the convergence of the pandemic and the Black Lives Matter movement — brings a unique opportunity.
The Aboriginal health sector’s response to the pandemic, faster and more effective than those from mainstream organisations, has been widely acknowledged. The role of the Aboriginal and Torres Strait Islander Advisory Group on Covid-19, which has been advising the Australian Health Protection Principal Committee, shows how tackling institutional racism through structural change can lead to better outcomes. The group, co-chaired by the National Aboriginal Community Controlled Health Organisation, or NACCHO, works on principles of shared decision-making, power sharing, two-way communication, self-determination, leadership and empowerment, according to a report in the Medical Journal of Australia.
Rallah-Baker, who is now president of the Australian Indigenous Doctors’ Association, or AIDA, says the Black Lives Matter movement has catapulted longstanding concerns into mainstream consciousness. “In Australia, we’ve had our own issues and debates around deaths in custody, and treaty, and reconciliation, right back to the Indigenous wars of independence,” he says. “By seeing those movements become mainstream in other Western countries, Australians start to question their own system.”
Weeks before our screens filled with the brutal images of a policeman’s knee on the late George Floyd’s neck, AIDA called out the racism Aboriginal and Torres Strait Islander people were experiencing in health services during the pandemic (for example, a patient who identified as an Aboriginal person was denied testing because priority treatment would only be offered to “real Aborigines”). AIDA also called for the early release of imprisoned First Nations people to prevent Black Covid-19 deaths in custody.
In April, the Australian Health Practitioner Regulation Agency backed AIDA’s concerns and encouraged Aboriginal and Torres Strait Islander people to lodge complaints if they had experienced racism or culturally unsafe care. “We will not tolerate racism particularly given the impact it has on community members accessing critical healthcare at this time,” said chief executive Martin Fletcher.
Just a few months later, non-Indigenous public health officials were warning Australians against attending Black Lives Matter marches, while remaining silent on public health threats such as police brutality and institutional racism. Indigenous health leaders spoke up strongly in response. The Centre of Best Practice in Aboriginal and Torres Strait Islander Suicide Prevention urged schools “to teach children about our history of racism, the social and historical determinants that underlie it, how this historical oppression continues, and what each of us can do to stand against racism.” NACCHO joined a broad coalition calling for the prime minister and opposition leader to support a bipartisan national anti-racism strategy.
Pat Anderson, chair of the Lowitja Institute, criticised the government’s lack of acknowledgement of the core concerns of Black Lives Matter. “We need to acknowledge that racism is deeply entrenched in Australia and is a public health emergency for Aboriginal and Torres Strait Islander people,” she said. But instead of taking urgent action on the Black Lives Matter concerns, “our government criticises us for our protests.”
In Melbourne, the chief executive officer of the Lowitja Institute, Narrunga Kaurna woman Janine Mohamed, a longstanding advocate for cultural safety, marched with her family and other colleagues working in Aboriginal health. As they walked, she later wrote, she thought about the linkages between punitive health and justice systems, and the stories of Ms Dhu, Naomi Williams, Tanya Day and David Dungay Junior and their preventable deaths. “So many of our people have been hurt and harmed by traumatising systems. Yet it took the death of an African-American man in the US to bring so many non-Indigenous Australians out on to the streets.”
At Wagga Wagga, in the NSW Riverina, Donna Murray, chief executive officer of Indigenous Allied Health Australia, joined hundreds of others in the Black Lives Matter march, where many wore masks and carried signs declaring “I can’t breathe.” She was moved by thoughts of the late Naomi Williams and her family, she tells me, and how little the mainstream health system had done to address the coroner’s findings. A descendant of the Wiradjuri nation of the Murrumbidgee River and of the Wonnarua nation of the Hunter Valley in New South Wales, Murray has spent decades working in Aboriginal and Torres Strait Islander affairs within government and community organisations.

What happens when all the non-Indigenous people go home? Indigenous Allied Health Australia’s Donna Murray. Honoring Nations/YouTube
On that day, she felt good to be on her Country and connecting with community after stressful months supporting members, many of whom were reporting increases in racism in their daily working and social lives as a result of the pandemic. “Fairly early on, it was quite obvious that it was going to be an issue to manage,” she says. Like other Aboriginal and Torres Strait Islander health workforce groups, her organisation ran webinars for members, stressing the importance of self-care and the cultural determinants of health as an antidote to racism.
Like Rallah-Baker, Murray believes that the increased global awareness arising from the pandemic and Black Lives Matter has created an opportunity to drive the anti-racism agenda. She would like a national process for tackling racism in health and education, including more support for Aboriginal and Torres Strait Islander people to make complaints about health services and health professionals.
She also wants non-Indigenous people and organisations to deal with racism. This is not the responsibility of Indigenous people and organisations, she says. “Our responsibility is to support our own people in caring for families and communities, and stay strong so we can keep identifying our priorities and find solutions through nation-building and self-determination.”
Murray suggests that I ask Speech Pathology Australia about why it came out in support of Black Lives Matter, one of a small number of mainstream health organisations to do so. When I question SPA national president Tim Kittel about this, he links the statement to other changes made by the organisation, including setting up an Aboriginal and Torres Strait Islander committee, making a formal apology to Aboriginal and Torres Strait Islander people for the profession’s history of causing harm, and encouraging members to undertake cultural safety training.
The SPA board is “firm” on the need to address the systemic discrimination and racism experienced by First Nations people, says Kittel. “There is so much more to do.”
At the end of the march in Wagga, Murray says she was left wondering: “When all those non-Indigenous people go home, what are they going to change and transform, so we don’t all have to keep coming back to march and speak out in another twelve months’ time, still in the same place, under the same dominant system? That’s always my question.”
Towards the end of a webinar hosted by the Australian Healthcare and Hospitals Association — coincidentally held the day after George Floyd was killed in Minneapolis — the AHHA’s strategic programs director, Chris Bourke, showed a complex “mud map” outlining multiple, overlapping ways that racism in healthcare is being dealt with through regulations and law.
It included the Australian Commission on Safety and Quality in Health Care’s implementation of new national healthcare standards released in 2017, race discrimination law, and the Australian Health Practitioner Regulation Agency’s work to embed cultural safety across healthcare.
Bourke, a Gamilaroi man, brings wide-ranging experience to this work, as Australia’s first Indigenous dentist and a member of the ACT Legislative Assembly from 2011 to 2016, where he held ministerial roles across portfolios including Aboriginal and Torres Strait Islander affairs, children and young people, disability, corrections, and education and training.
He says his father, an Aboriginal schoolteacher and principal, had a profound impact on his education. “I was incredibly lucky to be in such an environment and it protected myself and my siblings from many of the impacts of racism and discrimination that so many other Aboriginal and Torres Strait Islander people experience both in going to school and growing up.”
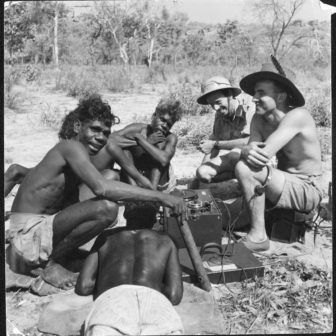
He studied dentistry because he liked science and doing things with his hands, and wanted to help people. He recalls working on Groote Eylandt in the Gulf of Carpentaria in the 1980s, when the dental clinic that served the non-Indigenous community was relatively well equipped but the one for local Aboriginal people “looked like something out of before the war.”
“There was no capability to do any fillings; you were there to take people’s teeth out. There wasn’t even an autoclave,” he recalls. “This was truly appalling — an example of a pattern of care, a model of care that’s been established as a result of institutional racism.”
Bourke says the concept of institutional racism recognises that organisations can serve some groups poorly because of the way they are run, managed, held accountable, resourced, located and staffed. It is about more than just staff behaviour, he says. Training and anti-racism courses will be ineffective if power structures don’t change.
Boards and management hold the key, but Bourke stresses the challenges involved. “It’s hard work. You have to play every note on the piano to get that change to happen.” But he is optimistic about “groundbreaking” developments in Queensland, where the state government, working with the Queensland Aboriginal and Islander Health Council and Indigenous academics, has drafted legislation to tackle institutional racism, including by requiring each hospital and health board to have at least one Aboriginal or Torres Strait Islander person as a member. With the pandemic constraining parliament’s operations, though, it’s not clear when the legislation will be debated, according to the office of Queensland health minister Steven Miles.
The South Australian health department is exploring a similar model, and is working with the AHHA on this. “That still leaves a number of other jurisdictions that could lean into this space and get some work done,” says Bourke.
In June last year, participants at the Lowitja Institute’s International Indigenous Health and Wellbeing Conference in Darwin outlined twelve priorities. “Colonialism and racism are determinants of ill health,” said one. “We call for comprehensive truth telling processes, and the acceptance of these truths, to dismantle colonial narratives and systemic racism in health research, policy and service delivery.”
While movements are growing for truth telling, as evidenced by the Uluru Statement from the Heart and, most recently, Victoria’s new truth and justice commission, the lived experience of many Aboriginal and Torres Strait Islander people shows a long road ahead.
__________
Tess Ryan writes:
Back in that waiting room I contemplate these developments, wearing all of my hats, including as president of the Australian Critical Race and Whiteness Studies Association.
My stomach churns reading again about Naomi Williams and her family. I think back to the time I spent with them, and the conversations we had about disconnections between cultural understandings of health and the health system. Recalling those days brings up all the anger and trauma, again. But this anger also fires us up to continue the fight.
We seem to be in a moment where change feels possible, and more commentary is recognising the many experiences of Black people and other people of colour. We are seeing very public denouncements of racism and an acknowledgement through numerous industries that those Black lives do matter. It is a powerful elixir to see allies also take on that work and young people in community wanting to carry the baton for changing these systems.
I want these developments to lead to systemic and structural change. It is the people within the system who need to see that change as necessary. At the micro or relationship level, I want to see behaviours shift in how we view various groups of people in connection with race. Rendering our bodies as statistical issues in health does nothing to change the paradigm of othering, and the focus on fixing the “condition” without having conversations about lived experience.
These developments are really only the beginning of the conversation we need to have. As an Aboriginal woman I will always want to work for that change, no matter how despondent I may feel. We look for the hope by looking backwards at all those who have advocated before us, and we look to the now and beyond in the strength of Black voices. We need to keep the momentum going, and for the policy changes to improve practice.
My hope is that I can walk into a medical clinic feeling like I am part of a team of people and professionals who will listen to my experiences, respect my different positions located in my identity, and work to build manageable solutions for better health and wellbeing. If I need a multidisciplinary team, then I expect them to work together with me and not sit in silos of their own discipline without connecting the dots to what can assist in better health.
I want to know that my mother is getting appropriate access to healthcare in her small town, that my brother doesn’t feel isolated from good health service delivery in a big city, and that a death like that of Naomi Williams won’t happen again. I want to see people like Kris Rallah-Baker supported and more Aboriginal and Torres Strait Islander people become ophthalmologists, or psychiatrists, or epidemiologists. We should see this as the norm and not the exception.
And I want other Australians to acknowledge and understand the hard work we do — as academics, professionals, policymakers, community members, commentators, digital media practitioners and artists — to try to educate you and open your eyes and ears and hearts. Our work, in navigating racism, informing people about discriminatory practice and working within institutional structures to create change, is immense.
We work to educate you in understanding difference, in pushing back against racial violence, in railing at the structures that think they can do better for us when we have our own solutions. Community-controlled health organisations have been doing exactly this during the pandemic, and these successes are regularly ignored.
Many Aboriginal and Torres Strait Islander people and communities have given decades of service to improve this country’s healthcare. It is time for other Australians to step up, take the responsibility and do the work, through your conversations and relationships as well as through changing policy and institutions and making yourselves accountable. We have been carrying you all this time without your even noticing. •
The publication of this article was supported by a grant from the Judith Neilson Institute for Journalism and Ideas.