Selling Our Souls: The Commodification of Hospital Care in the United States
By Adam D. Reich | Princeton University Press | $59.95
Hospitals are at once the providers of life-saving care, and big businesses. Their behaviour highlights the unresolved contradictions between the mission and the market, evident most vividly in the American healthcare system. These are the contradictions Adam Reich examines in Selling Our Souls.
The United States is unique among first world countries in the extent to which it has relied on the marketplace to determine the allocation of healthcare services. But these services are not simply commodities, and the failure to deliver them equitably has had consequences for individuals, the community and the nation. It was the growing cost of this marketplace failure that drove Barack Obama’s healthcare reforms. Here in Australia, the erosion of affordable access to universal healthcare and the new focus on competition in the guise of consumer choice could well lead to the very situation the United States is working to undo.
This book is about peculiarly American healthcare institutions seen through a distinctive American lens. The author is not a health-policy expert but a sociologist, and that perspective is evident in his approach. His focus is on just one aspect of the healthcare market – hospitals – at a time when the push is on to diminish their central, and expensive, role in the healthcare system in favour of expanded community-based care. Nevertheless, Reich provides useful insights for policy-makers in the United States and in Australia.
It is well recognised that enormous variations exist in hospital practices across the United States, but the reasons are poorly understood. Drawing on interviews and other fieldwork, Reich argues that the variations are not just a consequence of repertoires or cultures of practice but are also a manifestation of each hospital’s attempt to grapple with the contradictions inherent in the commodification of care. Selling Our Souls is as much about ethics, sociology and the social determinants of health as it is about emergency departments, operating theatres and clinicians’ remuneration.
Reich explores how three Californian hospitals founded at different times with different philosophical underpinnings and financing mechanisms – and consequently serving different patient populations – have responded to healthcare needs and market pressures. His thesis is that the three hospitals are “working, respectively, to rebuff, moralise, or tame a market that each regards as potentially undermining its core social commitment.” This affects the type of healthcare professionals each hospital attracts and their willingness and ability to deliver care to their patients.
Reich wrote his book during and after the enactment of Obamacare but before its implementation. It now needs to be read with a recognition of how healthcare reform is affecting acute care services by reducing the number of uninsured patients, creating new payment mechanisms and quality and safety initiatives, improving data reporting and transparency, and making increased use of electronic health records.
In selecting and categorising his three hospitals, Reich mirrors the major means by which most US hospitals are funded. Two-thirds of all urban American hospitals are non-profit. The remaining third is made up of for-profit and public hospitals, the latter often associated with medical schools. Sometimes Reich’s information and insights seem almost to have been selected to ensure that they firmly lock each hospital into its category, thus simplifying a very complicated world. Interestingly, though, Australia’s hospital system evolved in much the same way, with similar sponsorship and funding mechanisms.
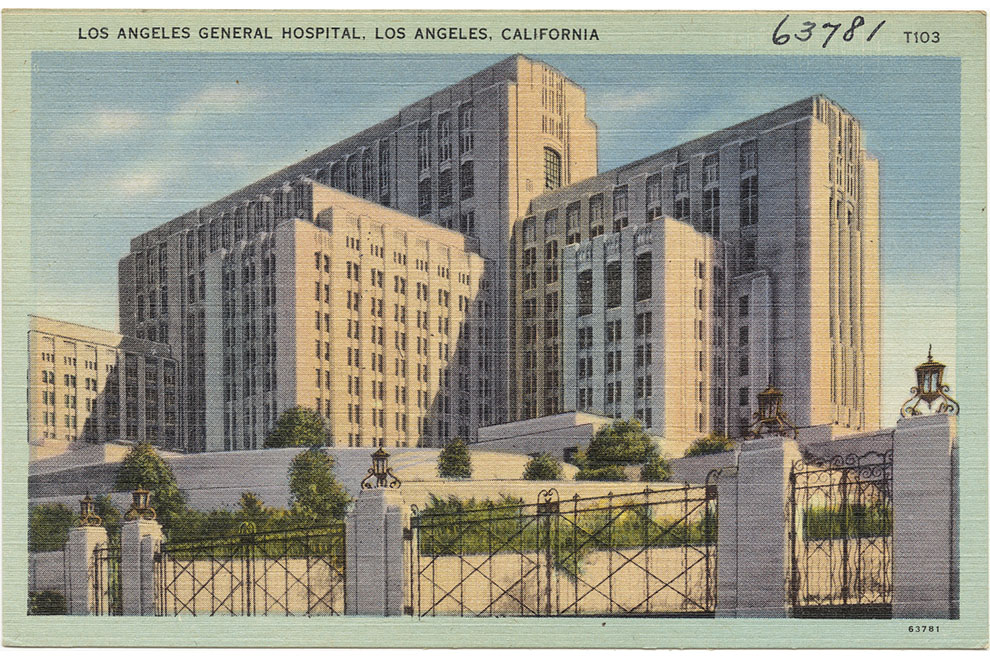
The first of Reich’s three hospitals, which he calls Publicare, was founded in the late nineteenth century to provide healthcare for the indigent. Today, its almshouse beginnings are echoed in its driving philosophy that everyone has a right to healthcare. It is a publicly funded teaching hospital, and many who work there believe that this contributes to its egalitarianism and what Reich describes as a “palpable camaraderie.”
Reich describes a commitment to the poor and underprivileged that is widely shared among the doctors and staff at PubliCare, who are more likely to see their professional identities in vocational terms than are their colleagues in the other hospitals, and also more likely to see the social dimensions to cases that elsewhere would be treated as purely medical problems. They worry about their patients and their needs beyond hospital care and struggle to reconcile the right to healthcare with care as a commodity to be sold.
This tension is particularly evident in the emergency department, which is frequently used by the poor, uninsured and under-insured for conditions that are not acute and aren’t always strictly medical. PubliCare staff need to be “resourceful in the face of a lack of resources” – both hospital resources and the lack of resources many patients bring with them.
PubliCare is the hospital that meets the needs of everyone in the community. In the face of a significant burden of uncompensated care it has several times come close to financial failure and resources are always tight. As described, PubliCare doesn’t directly match Australia’s public hospitals, but it does look like what our hospitals will become if Medicare is eroded and out-of-pocket costs continue to rise.
HolyCare hospital, Reich’s second exemplar, is owned by the Catholic Church. Its origins in the early part of the last century coincided both with the emergence of a middle class able to pay for care and with the establishment of hospitals as centres of medical authority and practice. When a market emerged for private hospital care as a way of enabling patients to distinguish themselves from the poor, benevolent organisations like the church responded, downplaying commerce and emphasising dignity and individualised treatment.
Reich discusses how hospitals like HolyCare have played a critical role in developing a “voluntary ideal” that protects patients from dehumanising public bureaucracy on the one hand and crass commercialisation on the other. In partnership with the medical profession, this approach has also delivered major revenues. Reich sees HolyCare’s efforts to imbue care with emotional and spiritual significance as giving some degree of moral legitimacy to highly entrepreneurial administrators and doctors.
It is interesting that staff relationships at HolyCare are seen as hierarchical and codified and that Reich felt that many people working there seemed miserable. It should be noted that he spent eight years working as a community organiser for workers’ rights in a Catholic hospital, and this has surely affected his thinking. But the environment at HolyCare is likely to be affected by its individual billing system, which means doctors have a clear incentive to see as many patients as possible and to compete for patients who can pay the highest rates. This leads to a disdain for the neediest patients that is in sharp contrast to the moral framework promulgated by the hospital administration.
The paradox is that the most explicitly spiritual hospital has the most individualistic and entrepreneurial doctors. Patient care is difficult to coordinate and there is a lack of integration and oversight of clinical practice. There are incentives for doctors to deliver more treatments than necessary – and they do. Both doctors and hospital share the financial rewards. Reich pointedly notes that much of the hospital’s “charity” is in fact the forgoing of inflated medical bills on which the hospital had been unable to collect.
To what extent are these observations about HolyCare reflected in Australia’s private hospitals, the majority of which are owned by Catholic Health? Private hospital patients mostly have private health insurance, but about a quarter of privately insured people choose to use the public health system. This may be because the care they need is only available in the public system, or it might reflect the out-of-pocket costs involved. In Australia the choice and advantages offered by private hospitals are often illusory.
The final hospital Reich examines is GroupCare. Because it is owned by a managed care organisation, it has its own clients, who are insured members of GroupCare Health System. Moreover, it is explicitly focused on bringing medical care into line with market norms. And in a further point of difference, while PubliCare and HolyCare are standalone facilities poorly integrated with primary care and specialist clinics, GroupCare hospital is deeply integrated with other facilities and resources in the GroupCare Health System.
With its focus on the efficient use of medical resources, GroupCare has a greater investment in ensuring patients’ chronic conditions are well-managed and expensive hospital costs are avoided; and it has the reach beyond the hospital doors to be able to do this. By catering to its own members, however, GroupCare largely ignores and excludes the uninsured.
Reich clearly sees GroupCare as having largely tamed the market through a “planned economy” approach that offers the most promising long-term possibility for containing the commodification of hospital care. But it’s also clear that he views this approach with great caution, worrying that rational care is inevitably rationed care. He expresses concern about the possibility of economic considerations infringing on the development of evidence-based protocols, although he indicates that existing protocols do not privilege economic considerations over medical ones.
There are intimations here of the arguments about “rationing” and “socialised medicine” that so poisoned the debate over Obamacare. This point is further highlighted by Reich’s finding that GroupCare is eliding the goal of maximising the health of each member with that of maximising the health of the membership as whole. But there is evidence to counter Reich’s fears. A recent study of non-profit hospitals that converted to for-profit shows improvements in their financial situation with no differences in quality or mortality rates or the proportion of poor or minority patients receiving care.
A case can be made that future healthcare reforms in Australia should aim to deliver something much closer to GroupCare than any other model. This hospital and others like it in the United States are working to rein in medical spending and improve health outcomes with an emphasis on population health rather than on isolated episodes of acute care. Of course there are trade-offs, but there are considerable gains to be made.
Reich highlights how GroupCare’s effective use of electronic health records allows for greater standardisation of treatment, monitoring and interaction with patients, and improved tracking of patient care. This wealth of information, together with a “culture of continuous improvement,” is used to improve physician care and patient involvement in that care.
Even if Reich’s overall formula for analysis is pat, he succeeds in bringing out the issues that are being debated in the United States and increasingly in Australia. The key element missing from his book is the voice of the healthcare consumer, who is entirely absent. That reflects the prime problem with the commodification of healthcare: it’s never about the patient. •