In the midst of an unfolding pandemic the crucial thing is to keep looking ahead. Taking lessons from steps we’ve already taken is good, but woulda, coulda, shoulda is a waste of time.
Victoria and New South Wales are experiencing significant surges of community transmission of Covid-19, the inevitability of which was signalled well in advance. And because detection is not perfect and restrictions of people’s movement across borders is not absolute, there is no guarantee this won’t spread to other states.
The techniques of widespread testing, contact tracing and isolation are now well practised, and may be enough to curb these outbreaks. But they may also prove insufficient, in which case further restrictions on people’s movement may be needed.
In this environment, criticisms of the COVIDSafe app as an expensive dud seem strikingly misplaced. The $2 million price tag is only a small morsel of chicken feed when stood against the accountancy error that recalculated the cost of the JobKeeper scheme from $130 billion to $70 billion. More to the point, COVIDSafe will only prove its worth if transmission grows so fast that human contact tracers are overwhelmed. Given that case notifications lag behind exposure events, in other words, those Australians who have not yet done so would be well advised to download the app.
This week’s public debate about “elimination” versus “aggressive suppression” has largely been beside the point. We now have enough data to know that Covid-19 spreads easily, including among young people. Closing down workplaces, public gatherings and educational institutions will reduce the chances of transmission. Confining whole populations to home will reduce transmission even further. Any level of active cases is enough to seed further outbreaks.
There is an analogy to be made with “sterilising immunity,” the ultimate goal of any perfect vaccine. The goal is to create an immune response sufficiently strong to prevent a virus from taking hold in a body. The problem with applying sterilising immunity to the body politic is that its outcomes may indeed be sterile. As philosopher Roberto Esposito has pointed out, immunity is the opposite of community, so the task is how to balance the two in a way that ensures community is not snuffed out.
With the spread of Covid-19 to nearly every nation and territory in the world, we have plenty of models from which to choose. The June outbreak in China, centred on Beijing’s Xinfadi wholesale produce market, was brought under control after 335 local transmission cases, but it took a vigorous effort including localised shutdowns and eleven million tests within a month.
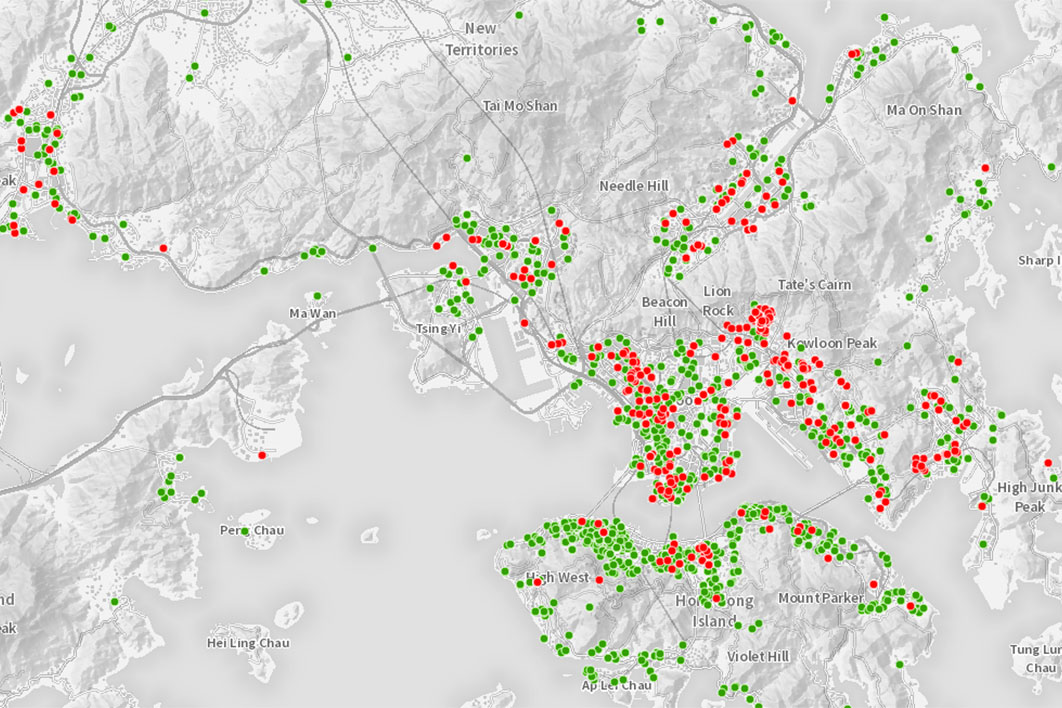
Hong Kong has entered what has been described as a third wave of infections, although the territory’s cumulative total of only 1400 cases means a daily spike into the teens is enough to register as a significant rise there. Hong Kong provides remarkably in-depth information about its Covid-19 cases: open up the map based on data from the territory government’s Centre for Health Protection and you’ll see identified cases right down to building level (as shown in the screenshot above).
Vietnam’s remarkable success deserves more comment, with a cumulative total of fewer than 400 cases and still no deaths. Most of the familiar elements are there: early, decisive action with border closures, quarantine, and school and workplace closures; and, over the longer term, extensive testing, active contact tracing and quarantine. Its contact-tracing model is perhaps the most telling: supported by a network of 700 district-level centres for disease control and more than 11,000 community health centres, contact tracing and attendant testing and isolation are routinely conducted for three degrees of separation: contacts of cases, contacts of contacts, and contacts of contacts of contacts.
Singapore remains perhaps the closest parallel to Australia. In July its daily number of new infections is closely paralleling Australia’s, and like Australia, it had initial success only to find that workers on the lowest economic rung, especially in close living quarters, were prime candidates for the virus. But, as the Anna Karenina principle would lead us to expect, there are important differences between the two countries’ experiences. An astounding 95 per cent of Singapore’s Covid-19 infections have been among migrant workers in dormitory blocks.
It’s these concentrations that have led Roland Bouffanais and Sun Sun Lim of the Singapore University of Technology and Design to suggest that much closer attention needs to be paid to “where the riskiest spots in the riskiest places — cities — might be.” This entails paying closer attention not only to places where people may gather for an extended time, but also to people’s behaviours when they’re gathered. It means attending to the differences between the mixing patterns of primary school children, who have a single set of classmates, and secondary students, who mix much more widely. It means using the datasets from phones, geolocated apps and public transport, and even from the people and vehicle flows collected by smart traffic lights, to build up a much more layered map of flows of people across cities.
Covid-19 control doesn’t come down to a binary choice between suppression and elimination. The settings need to be much more fine-grained than that. And to work so that communities are not alienated in the name of immunity, governments must make a much greater commitment to open information and participatory planning, alongside careful and detailed public health measures calibrated to risk.
Given the known risks of Covid-19 spread in abattoirs, for example, this should be an industry that only allows full-time employment with sick-leave entitlement, and all plants should have an in-house medical team. That might mean the end of cheap meat, but it seems an inevitable trade-off.
Workplace by workplace and block by block, we should expect Covid-19 risk to be incorporated into the pattern and rhythm of daily life. Against this benchmark, we ain’t seen nothing yet. •