SARS broke out in China’s Guandong province in November 2002. It spread to twenty-eight countries, infecting 8096 people and killing 774. By July 2003, though, the epidemic was over. In its 2006 report, SARS: How a Global Epidemic Was Stopped, the World Health Organization argued that the outbreak’s first lesson was that “we were lucky this time.” The reasons were simple: “If cases were infectious before symptoms appeared, or if asymptomatic cases transmitted the virus, the disease would have been much more difficult, perhaps even impossible, to control.”
In the last few weeks we have found out that Covid-19, a coronavirus with respiratory symptoms similar to SARS, can transmit before symptoms appear, and can be spread even by those who don’t eventually become sick. Luck, it seems, is against us this time.
A generation ago, infectious diseases were a medical backwater. Polio vaccination had been a stunning success: within a year of its licensing in 1955, the first of twenty-five million doses of the Salk vaccine had been produced by the Commonwealth Serum Laboratories and distributed across Australia. That last dreaded childhood disease was virtually eradicated, at least in countries with highly developed health systems. A combination of isolation and increasingly effective treatment also brought tuberculosis under control, and smallpox was well on the way to eradication: denied a home in its human hosts, it soon disappeared, and not even vaccination was needed any more.
The model seemed set. Virologists would get to work identifying viruses, and vaccines would be developed. Viral diseases dependent on human hosts would be pushed to extinction; bacterial diseases would be treated by antibiotics, increasingly powerful as needed, and intensive infection control.
By the late 1970s, modern medicine seemed to have vanquished the age-old threat of infectious disease. Extending these benefits to poorer countries with weak health systems was the only remaining challenge, but this was a task for do-gooder public health and development types, not the core business of high-prestige cutting-edge medicine.
But then, at the beginning of the 1980s, along came AIDS. Medicine was again faced with a disease it couldn’t cure and a pattern of transmission it didn’t understand. Layered on top of the standard waves of fear and stigma — the overblown fears of contagion and the obsessions with “patient zero” and super-spreaders — were fear and discomfort about its first sufferers, gay men, a new and still contested social category.
It didn’t take long, though, for the standard medical playbook to be deployed. AIDS had come to light in June 1981 when a cluster of unusual diseases among young gay men was reported in the US Centers for Disease Control’s Morbidity and Mortality Weekly Report. Less than three years later, in April 1984, US health and human services secretary Margaret Heckler convened a press conference where, alongside virologist Robert Gallo, she announced that the virus responsible for AIDS had been identified and along with it a blood test to “identify AIDS victims with essentially 100 per cent certainty.”
Heckler went on to assert that a vaccine would be developed within two years. Her confidence was misplaced: last month (on 3 February 2020, to be precise) the latest trial of the not-very-promising-but-most-promising-to-date HIV vaccine candidate was called off because infections in the vaccinated group were no lower than in the control group. The most optimistic forecasts for an effective HIV vaccine have now been pushed out to 2030 at the earliest.
With neither vaccine nor effective treatment available, HIV responses had to turn to social means — exposure avoidance, condom use, clean needles. Aided by various forms of denial and “othering,” HIV gradually developed into a full-blown global pandemic. But the effort to find treatments eventually paid off when it was discovered that antivirals that had been relatively ineffective when used alone could work in combinations of two or three. From 1996, effective HIV treatment was rolled out with an immediate impact on death rates.
The old problem of translating medical solutions to resource-poor settings once again reared its head, but this time a concerted global effort extended access even to the poorest countries within a few years. Antiviral treatment, it emerged, could not only stave off disease but also reduce the infectiousness of those with HIV. And when it was taken by uninfected people as prophylaxis, it could also prevent HIV acquisition. These treatment-driven solutions led to a resurgent triumphalism heralding “the end of AIDS.”
Modern medicine again reckoned itself to have won the fight against infectious disease. But it had only a few years to wait before the next potentially global epidemic appeared on the scene.
By February 2003, three months into the SARS epidemic, local health authorities had reported 305 cases and five deaths from atypical pneumonia of unknown cause. Cases spread to Hong Kong, Vietnam, Canada, Singapore and Taiwan. In March, a coronavirus was identified as the probable cause. By the end of that month, countries were considering travel bans. The World Health Organization started recommending against travel to affected areas, although every travel advisory was resisted by the countries named. Singapore and Hong Kong began imposing quarantine measures and closing schools. China’s response was initially slow, with Guangdong officials defensive, and only once SARS reached Beijing in April 2003 did it become a national priority. Full-scale infection control and quarantine measures were put in place and a national mobilisation launched under vice-premier Wu Yi.
As April turned to May, SARS was more or less under control. The last case found in Vietnam was on 7 April, and the WHO removed Vietnam from the list of affected countries on 28 April. By 5 July the last countries with local chains of transmission, Taiwan and China, were finally declared SARS-free.
China, in particular, learnt from SARS, and thoroughly overhauled its infectious disease control measures. The lack of transparency, reluctance to share information, and conflicts between local and central levels were widely perceived as failings, and China decided to transform itself into a paragon of public health virtue in the face of emerging epidemics by valuing shared information, acting decisively and openly, and cooperating globally.
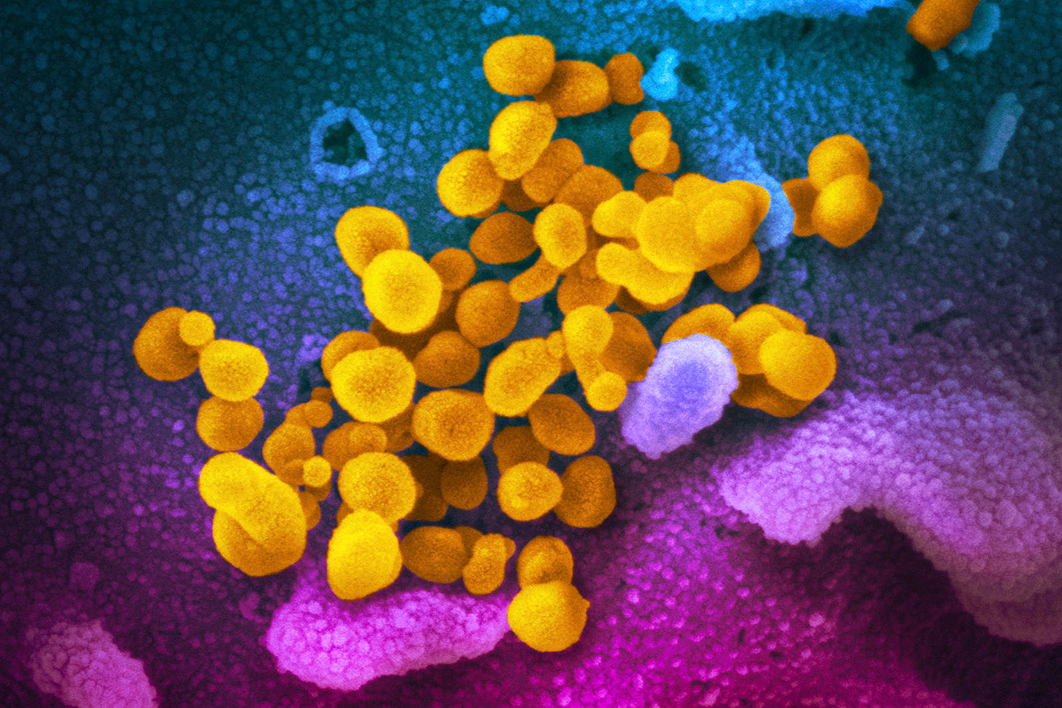
With new diseases now considered inevitable, a new paradigm focusing on health security began to emerge. Zoonoses were the most likely underlying cause — viruses jumping from animals to humans, with bats the most frequent originating culprit, often with an intermediate animal host. Population pressures, with more and more people crowded into newly expanding urban areas, were meanwhile creating susceptible locations for epidemic outbreak.
The 2013–16 West African Ebola epidemic was confirmation of the new paradigm. Previously, Ebola had emerged only in remote villages and seemed to be self-limiting. Because it was extremely infectious via body fluids, came on rapidly, and had visible symptoms and fatality rates between 50 and 90 per cent, an outbreak could be devastating locally but would burn itself out quickly. The 2013 outbreak was the first time Ebola had spread more extensively, into cities, across national borders and potentially across the globe. This epidemic’s almost 29,000 cases were a hundred times the number in previous Ebola outbreaks.
While international support for the affected West African countries was scandalously slow, it came eventually. The “global public good” of international health solidarity became an accepted norm. Health security was one of the few growth areas in Australia’s international development assistance portfolio under the Abbott–Turnbull government.

Contagion and its results: detail from Black Death At Tournai (1349) by Gilles Le Muisit. Bibliothèque Royale De Belgique
Quarantine, isolation and infection control
When the World Health Organization observed that the tools used successfully against SARS dated largely from the nineteenth century, it could equally have nominated the fourteenth century. Separating sick people from healthy ones had been a response to leprosy since biblical times. But it was not until the plague epidemics of the fourteenth century — the Black Death that swept across Europe and the Middle East — that clear notions of contagion and quarantine began to emerge.
When our descendants look back they are likely to place the intellectual culture of Moorish Al-Andalus among humanity’s high points. One of the outstanding figures of the final period of the Nasrid dynasty in Granada was the scholar and poet Ibn al-Khatib. After the devastating plague that struck the city and many others around the Mediterranean in 1348, he produced a short but keenly observed treatise on the Black Death, Muqni’at al-Sā’il ‘an al-Maraḍ al-Hā’il. Based on empirical observation, it included what is arguably medicine’s first precise account of contagion:
It becomes clear to anyone who has diagnosed or treated the disease that most of the individuals who have had contact with a plague victim will die, whereas the man who has had no exposure will remain healthy. A garment or vessel may carry infection into a house; even an earring can prove fatal to the man who has put it in his ear.
This account of contagion could have been put to good use in implementing effective infection control and quarantine measures at the time, but up until the mid nineteenth century the spread of disease was blamed mainly on vague notions of “miasmas” and putrefied air.
Responses to the Black Death did build on the model of sequestrated leper houses, though, and extended it to population movement in general, developing an elaborate codification of quarantine measures. Maritime cities in particular realised they were vulnerable to ship-borne plague.
In 1377 one of the Adriatic’s main maritime powers, Dubrovnik (known as Ragusa in Latin), introduced a requirement that ships from plague-affected areas be held in isolation for thirty days, and travellers from endemic or epidemic zones for forty days (hence the word quarantine) before they could enter the city. Venice, which had ruled Ragusa until 1358, established similar measures, designating a quarantine station on an island near the Lido in 1423, and other Mediterranean cities followed suit.
Even though Ragusa is credited with being the first to introduce a strict quarantine system, it was not completely successful. An outbreak in 1391 prompted even stricter regulations from 1397, but plague recurred in 1400 and again in 1416. When an outbreak in 1422 turned out to be very small, the measures were reckoned to at last be working.
Another wave of intense plague epidemics across Europe and England came in the mid seventeenth century. By now, elaborate public health apparatuses had been set up to respond with quarantine and isolation measures. Systems were particularly well developed in Italy, and the wealth of documentation that survived was mined brilliantly by Italian economic historian Carlo Cipolla. His fine-grained accounts of how cities like Prato, near Florence, responded to plague are uncanny premonitions of Covid-19 lockdowns in Lombardy today; and the anguish of inhabitants forcibly locked into houses and towns with plague sufferers parallels the experience of passengers and crew of the Diamond Princess.
Plague was not the only disease attracting a quarantine response. Syphilis was the “great pox” of the sixteenth century (as opposed to smallpox — “great” and “small” referring to the size of the pockmarks caused, not the severity of the epidemics). Later, cholera, yellow fever, typhoid and tuberculosis (the “white death”) provoked their own regimes of quarantine and isolation.
From the mid nineteenth century, though, quarantine began to lose its primacy, particularly after John Snow famously identified the contaminated pump handle at the centre of the Broad Street cholera outbreak in London in 1852. An understanding of germs, the precise targeting of infection sources, water purification and other sanitary measures, and the increasing use of vaccination proved effective in battling cholera. Quarantine began to be seen as a blunt, outdated instrument.
The disillusion stemmed partly from a conflation of quarantine, isolation and infection control. Isolation of sick patients and thorough disinfection are designed to definitively interrupt disease transmission. Quarantine seems to hold the same promise, but what needs to be understood is that it is fundamentally about probabilities, not absolutes.
The restriction of population movement by quarantine reduces the chances of exposure to the disease. How much it curbs epidemics depends on two things: how well the quarantine is kept, and the characteristic of the disease pathogen itself.
HIV was not a good candidate for quarantine because its years-long incubation period meant its spread was invariably well under way before it became evident. The cooperation of those who might have been exposed was therefore paramount. Stigma and quarantine are always antagonistic, but that didn’t stop a flurry of reactionary activism in 1992 by Bruce Shepherd, head of the Australian Medical Association, who darkly warned that the “gay lobby” had forced aside sensible public health measures. Shepherd was bouncing off remarks by the almost-sainted Fred Hollows that robust public health measures of identification and isolation of gay men were needed to protect Aboriginal communities from HIV.
A few countries tried to deal with AIDS on the model of tuberculosis sanatoria. But even that measure depended on persuading patients to accept a therapeutic embrace rather than be hunted down. That was Sweden’s initial approach, and that of Cuba when it was dealing with HIV in soldiers returning from supporting African liberation wars — the crucial factor being that these were returning heroes, not marginalised outsiders. Cuba has since gravitated to a more orthodox response, supportive and inclusive of gay men and sex workers. Credit for Cuba’s notably lower HIV rates compared with the rest of its region must also go to its highly effective public health system.

Intense focus: Deborah Birx, US coronavirus response coordinator (centre, left), and vice-president Mike Pence after a meeting on the epidemic with Republican senators yesterday. Andrew Harnik/AP Photo
Getting ahead of an epidemic
The lessons of stigma remain pertinent for Covid-19, although it has already become abundantly clear that it is futile to shun at-risk populations. On the contrary, the circumstances of transmission are all too familiar to all of us.
Particularly worrisome is the fact that transmission can readily occur before any signs of illness appear. Last week the Lancet published an account of one such transmission chain. A young woman passed through Wuhan by train on 21 January on the way to visit her family in Nanjing. There, she stayed with her sisters and mother and went to a family dinner on 23 January, before leaving for another city on 24 January. She had no symptoms until fever and a cough set in on 28 January, and she then tested positive to the coronavirus on 29 January. The immediate family with whom she stayed and three of the relatives at the dinner were subsequently found to be infected; two of the relatives at the dinner went to another family dinner the next day and three of the relatives at the latter dinner were diagnosed with the virus within two weeks.
The circumstances described in the Lancet allow for an unusually precise pinpointing of the timing and chain of transmission. But in every other way the report reveals what could well be happening at tens of thousands of family dinners in at least twenty countries.
“Most cases can still be traced to known contacts or clusters of cases,” the World Health Organization’s director-general, Tedros Adhanom, said at his briefing at the end of last week. “We do not see evidence as yet that the virus is spreading freely in communities. As long as that’s the case, we still have a chance of containing this virus, if robust action is taken to detect cases early, isolate and care for patients, and trace contacts.”
It is a universal rule that public health authorities always try to get ahead of epidemics. It is a near-universal fact that they rarely succeed. Covid-19 is still in the balance: the hopeful sign is that reported cases in China have been in steep decline since the end of January; the less hopeful sign is that significant chains of local transmission have erupted in at least twenty other countries.
New epidemics always seem to provide the opportunity to resurface old prejudices. A case in point is the “anonymous doctor” quoted in a slew of newspapers, including Sydney’s Sunday Telegraph, during the first wave of AIDS hysteria in 1982: “Perhaps we’ve needed a situation like this to demonstrate what we’ve known all along: depravity kills.”
Covid-19’s emergence in China just at a moment when the United States is ramping up its propaganda war against its biggest rival gave partisan commentators the opportunity to make outlandish claims about secrecy, cover-ups and the dire consequence of epidemic outbreak under authoritarian regimes. The reverse may well apply. One reason Covid-19 was identified at all is that public health systems with good disease surveillance are able to pick up unusual disease clusters and peer under the surface. More chaotic systems find it harder.
Once again, AIDS tells the story: the only reason AIDS was identified relatively early was because it affected young gay men who were not expected to be falling ill and dying. It depended on gay men as a category visible to the health system, and it depended on their illness being unusual. In fact, an epidemic of “junkie pneumonia” had been picked up in New York at least two years earlier, but deaths among drug users were not unusual, so no alarm bells rang. Similarly, the spread of AIDS in West Africa, predating the identification of the disease in the United States, disappeared into a background of high mortality.
When a schoolboy with no travel history or contact with known cases was diagnosed with Covid-19 in Washington State last week, his virus was genetically linked to that found in a man, recently returned from Wuhan, who had been identified on 19 January. The evidence points to a silent and untracked spread through the community over at least six weeks. The United States may yet prove one of the biggest challenges to the WHO’s hope of tracking and containing the virus.
Donald Trump’s appointment of vice-president Mike Pence to oversee the coronavirus response has been widely criticised, with many pointing to Pence’s dismal record in responding to a 2015 drug-use-driven HIV outbreak in Indiana when he was governor. In other circumstances, designating a vice-president to lead the response would have been taken as a sign of serious political commitment.
Muting the criticism was the swift and savvy appointment of Deborah Birx to the position of coronavirus response coordinator, reporting to Pence. Birx has been the US global AIDS coordinator since 2014, overseeing a US$7 billion annual budget. Her track record has been in classic public health containment and control, with an intense focus on understanding where the epidemic is, and a ruthless determination to spend available resources on targeted, evidence-based responses.
Buying time
New epidemics inevitably carry the burden of fear, prejudice, conspiracy theories and misinformation. But the brute reality of virus spread can be salutary. It creates an evolutionary pressure towards pragmatically effective responses, and heightens the stakes for the sifting of good information from bad.
The current state of play for Covid-19 suggests that China has been successful in containing the first wave of the epidemic in Wuhan and its surrounding province. The extent of asymptomatic transmission suggests that there may be a larger pool of infections than currently estimated, which means that succeeding waves of infection are likely, but may be smaller. It also means that the spread outside China has been extensive, and long chains of transmission seem inevitable in many, if not most, countries. Restrictions on travel, school closures and the cancelling of big public events will reduce transmission, but the challenge will be in balancing costs against benefits.
One implication of a larger-than-estimated pool of infections is that the case fatality rate may be much lower than the current 3.4 per cent figure. The virus may also weaken, and it may eventually be the case that most people with Covid-19 won’t even notice they have had the disease — much as they don’t notice the common coronaviruses that circulate widely and are at most associated with mild colds. But if anything like the current critical-illness rate of 5 per cent persists, then the burden on health systems will be huge.
One reason quarantine measures are still in place despite the evident breadth of spread is that they buy time. The best use of that time is coordinated global action. It is heartening that journals like the Lancet and publishers including Elsevier have established open-access repositories of the latest information.
The development of treatments and vaccines is also proceeding apace. The 2013–16 Ebola outbreak successfully pioneered vaccine trialling in the middle of an ongoing epidemic. Vaccine efforts ramped up quickly during the 2003 SARS epidemic, though unfortunately those efforts faded as the epidemic receded. This time around, vaccine efforts need to kick in as soon as possible — and be pursued until they reach success.
To the extent that the virus is brought under control it will be because of global cooperation, open and accurate communication, and development of widely accessible “public goods,” in this case vaccines and treatments. It seems like we might still need the “global community” after all. •